Hammer Toe Treatment Physical Therapy
Hammer toes and mallet toe are two foot deformities that occur most often in women who wear high heels or shoes with a narrow toe box. These types of footwear may force your toes against the front of the shoe, causing an unnatural bending. A hammertoe has an abnormal bend in the middle joint of a toe. Mallet toe affects the joint nearest the toenail. Hammertoe and mallet toe are most likely to occur in the toe next to your big toe. Relieving the pain and pressure of hammertoe and mallet toe may involve changing your footwear and wearing shoe inserts. If you have a more severe case of hammertoe or mallet toe, you may need surgery to experience relief.
Causes
Medical problems, such as stroke or diabetes that affect the nerves, may also lead to hammertoe. For example, diabetes can result in poor circulation, especially in the feet. As a result, the person may not feel that their toes are bent into unnatural positions. The likelihood of developing hammertoe increases with age and may be affected by gender (more common in women) and toe length; for example, when the second toe is longer than the big toe, hammertoe is more likely to occur. Hammertoe may also be present at birth. Genetics may factor in to developing hammertoe, particularly if the foot is flat or has a high arch, resulting in instability.
Symptoms include sharp pain in the middle of the toe and difficulty straightening the toe. People with hammertoe hammertoe may also develop blisters, which are fluid-filled pockets of skin, because the bent toe is likely to rub against the inside of a shoe. This increased friction may also lead to calluses, which are areas of thickened skin, and corns, which are hard lumps that may form on or between toes. Symptoms may be minor at first, but they can worsen over time.
Diagnosis
Some questions your doctor may ask of you include, when did you first begin having foot problems? How much pain are your feet or toes causing you? Where is the pain located? What, if anything, seems to improve your symptoms? What, if anything, appears to worsen your symptoms? What kind of shoes do you normally wear? Your doctor can diagnose hammertoe or mallet toe by examining your foot. Your doctor may also order X-rays to further evaluate the bones and joints of your feet and toes.
Non Surgical Treatment
Changing the type of footwear worn is a very important step in the treatment of hammer toes. When choosing a shoe, make sure the toe box (toe area) is high and broad, and can accommodate the hammer toes. A shoe with a high, broad toe box will provide enough room in the forefoot area so that there is less friction against the toes. Other conservative treatments include using forefoot products designed to relieve hammer toes, such as hammer toe crests and hammer toe splints. These devices will help hold down the hammer toe and provide relief to the forefoot. Gel toe shields and gel toe caps are also recommended to eliminate friction between the shoe and the toe, while providing comfort and lubrication.
Surgical Treatment
There are several surgical methods to correct a hammer toe. Your physician will decide which method will be most beneficial to you depending on the severity of your deformity, the direction the toe is deviating and the length of the affected toe. Some common surgical methods include. Arthroplasty. To promote straightening, half of the joint located directly underneath the crooked part of the toe is removed. Arthrodesis (fusion) To promote straightening, the joint directly underneath where the toe is crooked is completely removed. A wire or pin is inserted to aid healing. Tendon transfer. Performed alone or in combination with other procedures, a surgeon will take tendons from under the toe and ?re-route? them to the top of the toe to promote straightening. Basal phalangectomy. Performed to assist patients with severe stiffness, this procedure removes the base of the bone underneath the toe. Weil osteotomy. Performed to assist patients with severe stiffness, this procedure involves shortening the metatarsal bone and inserting surgical hardware to aid healing.
 Prevention
Prevention
You can avoid many foot, heel and ankle problems with shoes that fit properly. Here's what to look for when buying shoes. Adequate toe room. Avoid shoes with pointed toes. Low heels. Avoiding high heels will help you avoid back problems. Adjustability. Laced shoes are roomier and adjustable.
Over-Pronation Of The Feet What Are The Treatments
Overview
Overpronation and underpronation describe general foot movements. These terms do not necessarily describe a medical problem with a foot. For example, you can overpronate and not have any problems or symptoms at all. It is important to have your foot structure and symptoms adequately assessed by your prescribing physician and a qualified practitioner such as a Canadian Certified Pedorthist. Once the underlying conditions and mechanical faults are assessed, an appropriate treatment plan including possible orthotic and footwear recommendations can be made.
Causes
For those not familiar with the term pronation, you might be familiar with terms related to shoes and pronation such as ?motion control?, ?stability,? and ?neutral cushioned.? The terms motion control and stability are typically associated with the word ?over-pronation? or a foot that is supposedly pronating too much and needs correction. According to the running shoe industry, ?over-pronation? is a biomechanical affliction evident when the foot and or ankle rolls inward past the vertical line created by your leg when standing.
Symptoms
With over pronation, sufferers are most likely to experience pain through the arch of the foot. A lack of stability is also a common complaint. Over pronation also causes the foot to turn outward during movement at the ankle, causing sufferers to walk along the inner portion of the foot. This not only can deliver serious pain through the heel and ankle, but it can also be the cause of pain in the knees or lower back as well. This condition also causes the arch to sink which places stress on the bones, ligaments, and tendons throughout the foot. This may yield other common conditions of foot pain such as plantar fasciitis and heel spurs.
Diagnosis
Firstly, look at your feet in standing, have you got a clear arch on the inside of the foot? If there is not an arch and the innermost part of the sole touches the floor, then your feet are over-pronated. Secondly, look at your running shoes. If they are worn on the inside of the sole in particular, then pronation may be a problem for you. Thirdly, try the wet foot test. Wet your feet and walk along a section of paving and look at the footprints you leave. A normal foot will leave a print of the heel, connected to the forefoot by a strip approximately half the width of the foot on the outside of the sole. If you?re feet are pronated there may be little distinction between the rear and forefoot, shown opposite. The best way to determine if you over pronate is to visit a podiatrist or similar who can do a full gait analysis on a treadmill or using forceplates measuring exactly the forces and angles of the foot whilst running. It is not only the amount of over pronation which is important but the timing of it during the gait cycle as well that needs to be assessed.

Non Surgical Treatment
Get a gait analysis of your running style, this will highlight if you overpronate, oversupinate or have a neutral gait. Most podiatrists, physio's and sports therapists will offer this service, as do some specialist sports shops. Find a clinic. If you overpronate, get orthotics with extra medial support. Many running shoes have a harder material on the inside of the midsole (the thick hard foam part of the running shoe). This means the inside of the shoe will be compressed less under load and support the inside of the foot preventing it from rolling in or flattening. For people with considerable overpronation, another option is to have an orthotic device fitted. Orthotic insoles come in many types and prices. Some are pre-molded and can be bought off the shelf. These are ok for the majority of problem feet. However some cases may require specially casted orthotics from a relevant sports injury therapist or podiatrist.
Surgical Treatment
The MBA implant is small titanium device that is inserted surgically into a small opening between the bones in the hind-mid foot: the talus (ankle bone) and the calcaneus (heel bone). The implant was developed to help restore the arch by acting as a mechanical block that prevents the foot from rolling-in (pronation). In the medical literature, the success rate for relief of pain is about 65-70%. Unfortunately, about 40% of people require surgical removal of the implant due to pain.
Severs Disease Facts And Figures
Overview
Severs disease is pain in one or both heels when walking. The pain comes from the area between the sections of bone that make up the heel. As you go through a ?growth spurt? the tendon at the back of the heel (Achilles tendon) pulls at the heel bone. This makes you limp or walk on your toes and often creates a lump on your heel. The reason the tendon is tight is because your bones grow faster than your muscles. It usually affects boys between eight to ten years old, girls between ten and 12 years old, children in a ?growth spurt?, children involved in sports, usually those that involve running and jumping.
Causes
At birth, most of our foot bones are still made of cartilage, which ossifies (becomes bony) over the first few years of life. At the back of the heel, there is a growth plate that is attached to the main body of the heel bone by a cartilaginous join. At about the age of 14-15 years, this area of cartilage between the growth plate and the heel bone ossifies, fusing the area to the heel. Sever?s disease occurs when there is too much motion or strain across the growth plate, resulting in this area becoming inflamed and painful.
Symptoms
Sever's disease usually develops gradually. The pain from Sever's disease is often intermittent and localized to the area where the Achilles tendon attaches to the calcaneus. Swelling may be noted in this area. There can be tenderness on squeezing the calcaneus or pain when trying to stretch the calf muscles. Occasionally there is night pain. As Sever's disease progresses there can be continuous pain.
Diagnosis
Sever?s disease can be diagnosed based on the symptoms your child has. Your child?s doctor will conduct a physical examination by squeezing different parts of your child?s foot to see if they cause any pain. An X-ray may be used to rule out other problems, such as a broken bone or fracture.
Non Surgical Treatment
See a doctor, who can diagnose the injury and recommend appropriate treatment options. It will be beneficial to rest the affected heel, and to regularly ice the affected area for the first few days. Anti-inflammatory pain medication can reduce pain and swelling, but first check with your doctor. As the pain diminishes a physical therapist can assist with a program of rehabilitation, incorporating stretching and strengthening exercises focused on the calf, shin and hamstring muscles. For a period after the injury has healed the doctor may advise on changes to your training routines that seek to lessen the strain on the heels. Orthotics are often recommended for your shoes in order to correct any biomechanical problems or lend extra support to the heels.
Recovery
This condition is self limiting - it will go away when the two parts of bony growth join together - this is natural. Unfortunately, Sever's disease can be very painful and limit sport activity of the child while waiting for it to go away, so treatment is often advised to help relieve it. In a few cases of Sever's disease, the treatment is not successful and these children will be restricted in their activity levels until the two growth areas join - usually around the age of 16 years. There are no known long term complications associated with Sever's disease.
Flat Feet In Adults
Overview
Adult acquired flatfoot deformity (AAFD) is a painful, chronic condition found most often in women between the ages of 40 and 60. AAFD occurs when the soft tissues of the foot are overstretched and torn, causing the arch to collapse. Flatfoot deformities may also be caused by a foot fracture, or may result from long-term arthritis. Once the posterior tibial tendon-the tendon unit that holds up the arch-loses its function, the foot becomes flat as the bones spread out of position during weight bearing. Without an AAFD repair, the condition may progress until the affected foot becomes entirely rigid and quite painful.

Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot deformity. There is often no specific event that starts the problem, such as a sudden tendon injury. More commonly, the tendon becomes injured from cumulative wear and tear. Posterior tibial tendon dysfunction occurs more commonly in patients who already have a flat foot for other reasons. As the arch flattens, more stress is placed on the posterior tibial tendon and also on the ligaments on the inside of the foot and ankle. The result is a progressive disorder.
Symptoms
Many patients with this condition have no pain or symptoms. When problems do arise, the good news is that acquired flatfoot treatment is often very effective. Initially, it will be important to rest and avoid activities that worsen the pain.
Diagnosis
Observation by a skilled foot clinician and a hands-on evaluation of the foot and ankle is the most accurate diagnostic technique. Your Dallas foot doctor may have you do a walking examination (the most reliable way to check for the deformity). During walking, the affected foot appears more pronated and deformed. Your podiatrist may do muscle testing to look for strength deficiencies. During a single foot raise test, the foot doctor will ask you to rise up on the tip of your toes while keeping your unaffected foot off the ground. If your posterior tendon has been attenuated or ruptured, you will be unable to lift your heel off the floor. In less severe cases, it is possible to rise onto your toes, but your heel will not invert normally. X-rays are not always helpful as a diagnostic tool for Adult Flatfoot because both feet will generally demonstrate a deformity. MRI (magnetic resonance imaging) may show tendon injury and inflammation, but can?t always be relied on for a complete diagnosis. In most cases, a MRI is not necessary to diagnose a posterior tibial tendon injury. An ultrasound may also be used to confirm the deformity, but is usually not required for an initial diagnosis.
Non surgical Treatment
There are many non-surgical options for the flatfoot. Orthotics, non-custom braces, shoe gear changes and custom braces are all options for treatment. A course of physical therapy may be prescribed if tendon inflammation is part of the problem. Many people are successfully treated with non-surgical alternatives.

Surgical Treatment
For patients with a more severe deformity, or significant symptoms that do not respond to conservative treatment, surgery may be necessary. There are several procedures available depending on the nature of your condition. Ligament and muscle lengthening, removal of inflamed tendon lining, transferring of a nearby tendon to re-establish an arch, and bone realignment and fusion are examples of surgical options to help with a painful flatfoot condition. Surgery can be avoided when symptoms are addressed early. If you are feeling ankle pain or notice any warmth, redness or swelling in your foot, contact us immediately. We can create a tailored treatment plan to resolve your symptoms and prevent future problems.
What Will Cause Achilles Tendonitis ?
Overview
 Do you experience dull pain near the back of your heel or in the back of your leg after your regular run or after playing your favourite sport? When you ramp up your exercise is the pain more severe or prolonged? If so, you may have Achilles tendinitis. The Achilles tendon is the thick, strong, springy band of tissue that connects the muscles from the middle of your calf to your heel bone. You use your Achilles tendon when you walk, run or jump. Achilles tendinitis occurs when the Achilles tendon is repeatedly strained. The Achilles tendon becomes less flexible, weaker and more prone to injury as we age. Middle-aged weekend warriors and runners who suddenly intensify their training often suffer from Achilles tendinitis.
Do you experience dull pain near the back of your heel or in the back of your leg after your regular run or after playing your favourite sport? When you ramp up your exercise is the pain more severe or prolonged? If so, you may have Achilles tendinitis. The Achilles tendon is the thick, strong, springy band of tissue that connects the muscles from the middle of your calf to your heel bone. You use your Achilles tendon when you walk, run or jump. Achilles tendinitis occurs when the Achilles tendon is repeatedly strained. The Achilles tendon becomes less flexible, weaker and more prone to injury as we age. Middle-aged weekend warriors and runners who suddenly intensify their training often suffer from Achilles tendinitis.
Causes
Achilles tendinitis usually results from overuse and not a specific injury or trauma. When the body is subject to repetitive stress, the Achilles tendon is more prone to become inflamed. Other factors may cause Achilles tendinitis, such as, Sudden increase in physical activity, which can be related to distance, speed or hills, without giving yourself adequate time to adjust to the heightened activity. With running up hills, the Achilles tendon has to stretch more for each stride, which creates rapid fatigue. Inadequate footwear or training surface. High heels may cause a problem, because the Achilles tendon and calf muscles are shortened. While exercising in flat, athletic shoes, the tendon is then stretched beyond its normal range, putting abnormal strain on the tendon. Tight calf muscles which gives the foot a decreased range of motion. The strained calf muscles may also put extra strain on the Achilles tendon. Bone spur where the Achilles tendon attaches to the heel bone, aggravating the tendon and causing pain.
Symptoms
Paratenonitis presents in younger people. Symptoms start gradually and spontaneously. Aching and burning pain is noted especially with morning activity. It may improve slightly with initial activity, but becomes worse with further activity. It is aggravated by exercise. Over time less exercise is required to cause the pain. The Achilles tendon is often enlarged, warm and tender approximately 1 to 4 inches above its heel insertion. Sometimes friction is noted with gentle palpation of the tendon during ankle motion. Tendinosis presents similarly but typically in middle-aged people. If severe pain and limited walking ability are present, it may indicate a partial tear of the tendon.
Diagnosis
A doctor examines the patient, checking for pain and swelling along the posterior of the leg. The doctor interviews the patient regarding the onset, history, and description of pain and weakness. The muscles, tissues, bones, and blood vessels may be evaluated with imaging studies, such as X-ray, ultrasound, or MRI.
Nonsurgical Treatment
Treatment can range from cold compress and heel pads for minor cases, to physical rehabilitation, anti-inflammatory medicine, ultrasound therapy, and manual therapy. If you are a Michigan resident that suspects they have Achilles Tendinitis, please contact Dr. Young immediately; Achilles Tendinitis, if left untreated, can eventually result in an Achilles Tendon Rupture, which is a serious condition that is a partial or complete tear in the tendon. It can severely hinder walking and can be extremely painful and slow to recover.

Surgical Treatment
It is important to understand that surgery may not give you 100% functionality of your leg, but you should be able to return to most if not all of your pre-injury activities. These surgical procedures are often performed with very successful results. What truly makes a difference is your commitment to a doctor recommended rehabilitation program after surgery as there is always a possibility of re-injuring your tendon even after a surgical procedure. One complication of surgical repair for Achilles tendon tear is that skin can become thin at site of incision, and may have limited blood flow.
Prevention
If you're just getting started with your training, be sure to stretch after running, and start slowly, increasing your mileage by no more than 10% per week. Strengthen your calf muscles with exercises such as toe raises. Work low-impact cross-training activities, such as cycling and swimming, into your training.
Complications Involving Diabetic Feet
Charcot joint (also known as charcot arthritis) is caused by the ankle and foot having poor sensation as a result of diabetes. This can cause small fractures to occur in the food and ankle, leading to pain in the foot bones. The term arthritis basically means a condition that affects the joints, which can subsequently result in joint pain or even stiffness in that particular area of the body.

The delayed- or non-healing of wounds is one of the major diabetes complications that cause suffering in people with diabetes and results in more than 500,000 new diabetic foot ulcers and 50,000 lower extremity amputations per year in the US alone. University of Notre Dame researchers have, for the first time, identified the enzymes that are detrimental to diabetic wound healing and those that are beneficial to repair the wound. On the other hand, type 2 diabetes is said to occur in middle-aged and the elderly, who suffer from problems in relation to obesity. Though most women experience these symptoms, in many cases, people suffering from type II diabetes do not experience any symptom for years. Usually, type 2 diabetes is diagnosed after serious health problems, like heart attacks, or vision problems arise. The International Symposium on the Diabetic Foot has become the standard international (scientific) meeting on this topic.
The infected bone may be very painful, and the skin above the bone can become red and swollen. The Cleveland Clinic explains that many diabetics experience a patchy loss of bone in their fingers, feet and toes. People with type 1 diabetes (which is also known as childhood diabetes and affects patients early in their lives) also have an increased risk of osteoporosis. As the bones get more brittle they become prone to miniature fractures, which may not be as obvious as a complete fracture but which can cause severe bone pain nonetheless.
Diabetic foot ulcers as one of the most common complications of diabetes mellitus are defined as nonhealing or long-lasting chronic skin ulcers in diabetic patients. Low level laser therapy (LLLT) on wound areas as well as on acupuncture points, as a noninvasive, pain-free method with minor side effects, has been considered as a possible treatment option for the diabetic foot syndrome. The majority of clinical studies show a potential benefit of LLLT in wound healing of diabetic ulcers.
Check shoes before they are put on the feet to make sure there are no rocks or objects inside of the shoes. Diabetics who have a loss of feeling in the feet may not be able to feel objects inside shoes, even when they are causing harm to the feet. You may have serious foot problems, but feel no pain.
Dyshidrotic eczema, which is also called vesicular eczema of hands or feet, is a form of eczema that is characterized by cracked skin and itchy blisters. The affected individual Flat Feet must refrain from scratching over the affected skin. Psoriasis is a skin condition that is characterized by the development of inflamed patches of skin and silvery scales.
What Triggers Plantar Fasciitis And Ways To Successfully Treat It

Overview
The plantar fascia (a connective tissue structure) stretches from the toes and ball of the foot, through the arch, and connects to the heel bone in three places: outside, center and inside. Normally it helps the foot spring as it rolls forward. It also provides support for the arch of the foot. The plantar fascia helps keep the foot on track, cutting down on oscillation. When the foot over-pronates (rolls to the inside) the plantar fascia tries to stabilize it and prevent excessive roll. In time, the inside and sometimes center connections are overstressed and pull away from their attachments. The first sign is usually heel pain as you rise in the morning. When you walk around, the pain may subside, only to return the next morning. Inflammation and increased soreness are the results of long-term neglect and continued abuse. A heel bone spur may develop after a long period of injury when there is no support for the heel. The plantar fascia attaches to the heel bone with small fibers. When these become irritated they become inflamed with blood containing white blood cells. Within the white blood cells are osteoblasts which calcify to form bone spurs and calcium deposits. The body is trying to reduce stress on that area by building a bone in the direction of stress. Unfortunately, these foreign substances cause pain and further irritation in the surrounding soft tissue.
Causes
Plantar fasciitis is caused by straining the ligament that supports your arch. Repeated strain can cause tiny tears in the ligament. These can lead to pain and swelling. This is more likely to happen if your feet roll inward too much when you walk, you have high arches or flat feet. You walk, stand, or run for long periods of time, especially on hard surfaces. You are overweight. You wear shoes that don't fit well or are worn out. You have tight Achilles tendons or calf muscles.
Symptoms
The symptoms of plantar fasciitis include pain in the bottom of your foot, especially at the front or centre of the heel bone, pain that is worse when first rising in the morning (called "first-step pain"), when first standing up after any long period of sitting, or after increased levels of activity especially in non-supportive shoes. Seek medical advice about plantar fasciitis if you have heel pain or pain in the bottom of your foot, especially when you get up in the morning, that does not respond to treatment or if there is redness or bruising in the heel.
Diagnosis
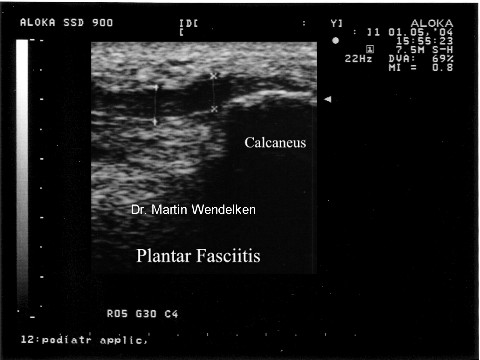
Your doctor can usually diagnose plantar fasciitis just by talking to you and examining your feet. Rarely, tests are needed if the diagnosis is uncertain or to rule out other possible causes of heel pain. These can include X-rays of the heel or an ultrasound scan of the fascia. An ultrasound scan usually shows thickening and swelling of the fascia in plantar fasciitis.
Non Surgical Treatment
Stabilize the foot by using uniquely placed wedges, deep heel cups, and "posts" (stabilizers). When the foot is stabilized, it is brought back to a neutral or normal alignment. When the foot is in its normal alignment, pronation and supination are reduced or completely corrected, and the abnormal pull on the Plantar Fascia is alleviated. This will allow the Plantar Fascia to begin to heal. When healing occurs, the pain and inflammation gradually subside. Provide the specific amount of arch support that your foot requires. Our custom-made orthotics support not only the arch as a whole, but each individual bone and joint that forms the arch. Whether your arch is flat or abnormally high, our custom-made orthotics will provide the support that you need. When the arch is properly supported, the Plantar Fascia is protected and healing can begin. Aid in shock absorption. The primary shock absorbers of our feet, and therefore our body, are the Plantar Fascia and the arch. To aid these structures, we construct our custom-made orthotics so that they provide semi-flexible support to the arch by "giving" to absorb the shock of each step, rather than our foot absorbing the shock (our orthotics act in the same way a shock absorber does on an automobile). When your weight is removed from the orthotic, the arch returns to its original height since the material we use has a built-in "memory." This action will help to keep the Plantar Fascia and arch healthy and pain free. Cushion the heel. Our custom-made orthotics use thin, cushiony, durable, materials to cushion and protect the heel. This helps to alleviate painful heels.
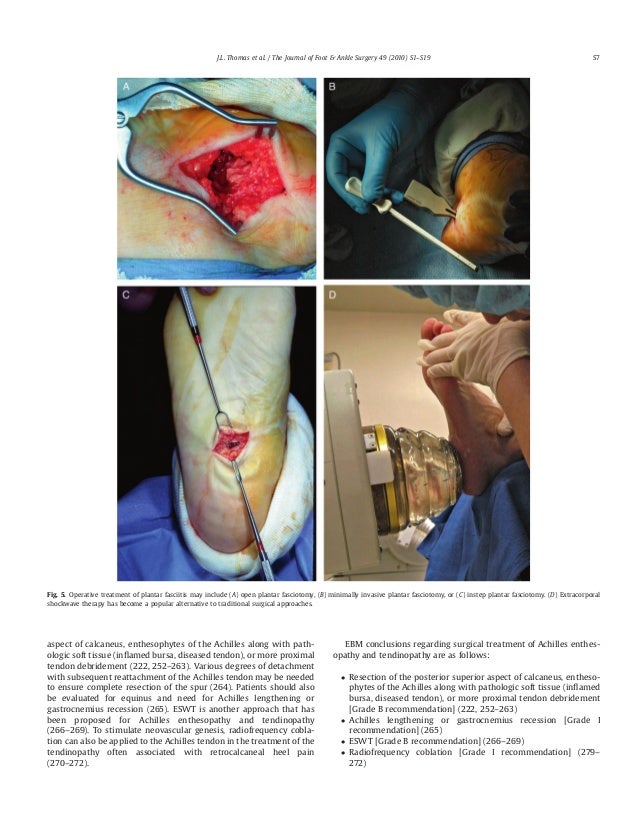
Surgical Treatment
Most studies indicate that 95% of those afflicted with plantar fasciitis are able to relieve their heel pain with nonsurgical treatments. If you are one of the few people whose symptoms don't improve with other treatments, your doctor may recommend plantar fascia release surgery. Plantar fascia release involves cutting part of the plantar fascia ligament in order to release the tension and relieve the inflammation of the ligament. Overall, the success rate of surgical release is 70 to 90 percent in patients with plantar fasciitis. While the success rate is very high following surgery, one should be aware that there is often a prolonged postoperative period of discomfort similar to the discomfort experienced prior to surgery. This pain usually will abate within 2-3 months. One should always be sure to understand all the risks associated with any surgery they are considering.
Prevention
To reduce your risk of getting plantar fasciitis take these steps. Wear appropriate and well-fitted footwear during sports and exercise. Do stretching exercises for the Achilles tendon and plantar fascia. Increase the intensity and duration of exercise gradually. Maintain an appropriate weight.
What Triggers Heel Pain And Approaches To Overcome It

Overview
The plantar fascia (a connective tissue structure) stretches from the toes and ball of the foot, through the arch, and connects to the heel bone in three places: outside, center and inside. Normally it helps the foot spring as it rolls forward. It also provides support for the arch of the foot. The plantar fascia helps keep the foot on track, cutting down on oscillation. When the foot over-pronates (rolls to the inside) the plantar fascia tries to stabilize it and prevent excessive roll. In time, the inside and sometimes center connections are overstressed and pull away from their attachments. The first sign is usually heel pain as you rise in the morning. When you walk around, the pain may subside, only to return the next morning. Inflammation and increased soreness are the results of long-term neglect and continued abuse. A heel bone spur may develop after a long period of injury when there is no support for the heel. The plantar fascia attaches to the heel bone with small fibers. When these become irritated they become inflamed with blood containing white blood cells. Within the white blood cells are osteoblasts which calcify to form bone spurs and calcium deposits. The body is trying to reduce stress on that area by building a bone in the direction of stress. Unfortunately, these foreign substances cause pain and further irritation in the surrounding soft tissue.
Causes
Currently no single factor has been reliably identified as contributing to the development of plantar fasciitis. The two risk factors with the most support from current research. Decreased ankle dorsiflexion. Increased Body Mass Index (BMI) in non-athletic populations. These factors are related in that both lead to increased strain on the arch, both lead to increased compression on the heel. When dorsiflexion range of motion (ankle flexibility) is lacking, the body compensates by increasing movement of the arch. In this way, decreased ankle dorsiflexion influences pronation and places strain on the underside of the foot. Similarly, having a high BMI causes strain because it places a load on the foot that may be in excess of what the foot can support. As mentioned earlier, overpronation is thought to be a contributing factor, but studies on this have so far produced mixed results. The second way these factors relate to each other is in the way people stand. A lack of ankle flexibility and a high BMI can both cause increased pressure on the heel in standing. Keeping weight on the heels causes compression under the heel. But it also means the muscles and ligaments in the arch are not being used to balance your body weight. Lack of use, I suspect, is a greater danger than overuse. Looking beyond these potential contributors to heel pain though, there is one major factor that overshadows them all-the way footwear alters the normal function of the foot.
Symptoms
The most obvious symptom of plantar fasciitis is a sharp pain on the bottom of the foot, near the heel. Here are some signals that this pain may be plantar fasciitis. The pain is strongest first thing in the morning but gets better after a few minutes of walking around. The pain is worse after standing for a long time or after getting up from sitting. The pain develops gradually and becomes worse over time. The pain is worse after exercise or activity than it is during activity. It hurts when stretching the foot. It hurts when pressing on the sides of the heel or arch of the foot.
Diagnosis
If you see a doctor for heel pain, he or she will first ask questions about where you feel the pain. If plantar fasciitis is suspected, the doctor will ask about what activities you've been doing that might be putting you at risk. The doctor will also examine your foot by pressing on it or asking you to flex it to see if that makes the pain worse. If something else might be causing the pain, like a heel spur or a bone fracture, the doctor may order an X-ray to take a look at the bones of your feet. In rare cases, if heel pain doesn't respond to regular treatments, the doctor also might order an MRI scan of your foot. The good news about plantar fasciitis is that it usually goes away after a few months if you do a few simple things like stretching exercises and cutting back on activities that might have caused the problem. Taking over-the-counter medicines can help with pain. It's rare that people need surgery for plantar fasciitis. Doctors only do surgery as a last resort if nothing else eases the pain.
Non Surgical Treatment
Plantar fasciitis is usually controlled with conservative treatment. Following control of the pain and inflammation an orthotic (a custom made shoe insert) will be used to stabilize your foot and prevent a recurrence. Over 98% of the time heel spurs and plantar fasciitis can be controlled by this treatment and surgery can be avoided. The orthotic prevents excess pronation and prevents lengthening of the plantar fascia and continued tearing of the fascia. Usually a slight heel lift and a firm shank in the shoe will also help to reduce the severity of this problem. The office visit will be used for careful examination and review to distinguish plantar fasciitis and plantar heel pain syndrome from other problems, many of which are outlined below. It is important to distinguish between a stress reaction of the calcaneus and plantar fasciitis. A feature of many calcaneal stress fractures is pain on lateral and medial compression of the calcaneus.

Surgical Treatment
Most patients have good results from surgery. However, because surgery can result in chronic pain and dissatisfaction, it is recommended only after all nonsurgical measures have been exhausted. The most common complications of release surgery include incomplete relief of pain and nerve damage.
What Is Heel Pain
Overview
Plantar fasciitis is one of the most common explanations of heel pain. It is caused by inflammation to the thick band that connects the toes to the heel bone, called the plantar fascia, which runs across the bottom of your foot. The condition is most commonly seen in runners, pregnant women, overweight people, and individuals who wear inadequately supporting shoes. Plantar fasciitis typically affects people between the ages of 40 and 70.
Causes
Plantar fasciitis is common in sports which involve running, dancing or jumping. Runners who overpronate where their feet roll in or flatten too much are particularly at risk the plantar fascia is over stretched as the foot flattens. A common factor is tight calf muscles which lead to a prolonged or high velocity pronation or rolling in of the foot. This in turn produces repetitive over-stretching of the plantar fascia leading to possible inflammation and thickening of the tendon. As the fascia thickens it looses flexibility and strength. Other causes include either a low arch called pes planus or a very high arched foot known as pes cavus. Assessing the foot for plantar fasciitisExcessive walking in footwear which does not provide adequate arch support has been attributed. Footwear for plantar fasciitis should be flat, lace-up and with good arch support and cushioning. Overweight individuals are more at risk of developing plantar fasciitis due to the excess weight impacting on the foot.
Symptoms
The main symptom of plantar fasciitis is heel pain when you walk. You may also feel pain when you stand and possibly even when you are resting. This pain typically occurs first thing in the morning after you get out of bed, when your foot is placed flat on the floor. The pain occurs because you are stretching the plantar fascia. The pain usually lessens with more walking, but you may have it again after periods of rest. You may feel no pain when you are sleeping because the position of your feet during rest allows the fascia to shorten and relax.
Diagnosis
The health care provider will perform a physical exam. This may show tenderness on the bottom of your foot, flat feet or high arches, mild foot swelling or redness, stiffness or tightness of the arch in the bottom of your foot. X-rays may be taken to rule out other problems.
Non Surgical Treatment
Careful attention to footwear is critical. Every effort should be made to wear comfortable shoes with proper arch support, fostering proper foot posture. Should arch supports prove insufficient, an orthotic shoe should be considered. Fortunately, most cases of plantar fasciitis respond well to non-operative treatment. Recovery times however vary enormously from one athlete to another, depending on age, overall health and physical condition as well as severity of injury. A broad period between 6 weeks and 6 months is usually sufficient for proper healing. Additionally, the mode of treatment must be flexible depending on the details of a particular athlete’s injury. Methods that prove successful in one patient, may not improve the injury in another. Early treatment typically includes the use of anti-inflammatory medication, icing, stretching activities, and heel inserts and splints. Cortisone injections may be necessary to achieve satisfactory healing and retard inflammation. In later stages of the rehabilitation process, typically after the first week, ice should be discontinued and replaced with heat and massage.

Surgical Treatment
Plantar fasciotomy is often considered after conservative treatment has failed to resolve the issue after six months and is viewed as a last resort. Minimally invasive and endoscopic approaches to plantar fasciotomy exist but require a specialist who is familiar with certain equipment. Heel spur removal during plantar fasciotomy has not been found to improve the surgical outcome. Plantar heel pain may occur for multiple reasons and release of the lateral plantar nerve branch may be performed alongside the plantar fasciotomy in select cases. Possible complications of plantar fasciotomy include nerve injury, instability of the medial longitudinal arch of the foot, fracture of the calcaneus, prolonged recovery time, infection, rupture of the plantar fascia, and failure to improve the pain. Coblation (TOPAZ) surgery has recently been proposed as alternative surgical approaches for the treatment of recalcitrant plantar fasciitis.
Stretching Exercises
While it's typical to experience pain in just one foot, massage and stretch both feet. Do it first thing in the morning, and three times during the day. Achilles Tendon Stretch. Stand with your affected foot behind your healthy one. Point the toes of the back foot toward the heel of the front foot, and lean into a wall. Bend the front knee and keep the back knee straight, heel firmly planted on the floor. Hold for a count of 10. Plantar Fascia Stretch. Sit down, and place the affected foot across your knee. Using the hand on your affected side, pull your toes back toward your shin until you feel a stretch in your arch. Run your thumb along your foot--you should feel tension. Hold for a count of 10.
What Is Heel Discomfort

Overview
Plantar fasciitis is a painful condition affecting the connective tissue that stretches between the heel and the middle of the foot. It is usually caused by overuse, injury or muscular abnormalities. In extracorporeal shockwave therapy, a machine is used to deliver sound waves to the painful area. It is not known exactly how it works, but it is thought that it might stimulate healing of the fascia.
Causes
A number of factors can contribute to plantar fasciitis. While men can get plantar fasciitis, it is more common in women. You're also more likely to have this condition as you age or if you are overweight. Take up a new form of exercise or suddenly increase the intensity of your exercise. Are on your feet for several hours each day. Have other medical conditions such as rheumatoid arthritis or lupus (systemic lupus erythematosus). Tend to wear high-heeled shoes, and then switch abruptly to flat shoes. Wear shoes that are worn out with weak arch supports and thin soles. Have flat feet or an unusually high arch. Have legs of uneven lengths or an abnormal walk or foot position. Have tight achilles tendons, or ‘heel cords’.
Symptoms
Plantar fasciitis has a few possible symptoms. The symptoms can occur suddenly or gradually. Not all of the symptoms must be present at once. The classic symptom of plantar fasciitis is pain around the heel with the first few steps out of bed or after resting for a considerable period of time. This pain fades away a few minutes after the feet warm up. This symptom is so common that it symbols the plantar fasciitis disorder. If you have it then probably you have plantar fasciitis. If you don’t suffer from morning pain then you might want to reconsider your diagnosis. Pain below the heel bone at the connection of the bone to the fascia. As the condition becomes more severe the pain can get more intense during the day without rest. Plantar fasciitis symptoms include pain while touching the inside of the heel or along the arch. Foot pain after you spend long periods of time standing on your feet. Pain when stretching the plantar fascia. Foot pain that worsens when climbing stairs or standing on the toes. Pain that feels as though you are walking on glass. Pain when you start to exercise that gets better as you warm up but returns after you stop.
Diagnosis
Most cases of plantar fasciitis are diagnosed by a health care provider who listens carefully to your description of symptoms. During an examination of your feet, your health care provider will have to press on the bottom of your feet, the area most likely to be painful in plantar fasciitis. Because the pain of plantar fasciitis has unique characteristics, pain upon rising, improvement after walking for several minutes, pain produced by pressure applied in a specific location on your foot but not with pressure in other areas, your health care provider will probably feel comfortable making the diagnosis based on your symptoms and a physical examination. Your health care provider may suggest that you have an X-ray of your foot to verify that there is no stress fracture causing your pain.
Non Surgical Treatment
Reducing inflammation in the plantar fascia ligament is an important part of treatment, though this does not address the underlying damage to the ligament. Initial home treatment includes staying off your feet and applying ice for 15 to 20 minutes three or four times a day to reduce swelling. You can also try reducing or changing your exercise activities. Using arch supports in your shoes and doing stretching exercises may also help to relieve pain. Nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen (i.e. Motrin or Advil) and naproxen (i.e. Aleve), are often used to reduce inflammation in the ligament. If home treatments and over-the-counter anti-inflammatory drugs don’t ease the pain, an injection of a corticosteroid directly into the damaged section of the ligament can be given. Your doctor can do this in his or her office. Your doctor may use an ultrasound device to help determine the best place for the injection. Corticosteroids can also be administered on the skin of your heel or the arch of your foot, and then a painless electrical current is applied to let the steroid pass through your skin and into the muscle. Physical therapy is an important part of treatment for planter fasciitis. It can help stretch your plantar fascia and Achilles tendons. A physical therapist can also show you exercises to strengthen your lower leg muscles, helping to stabilize your walk and lessen the workload on your plantar fascia. If pain continues and other methods aren’t working, your doctor may recommend extracorporeal shock wave therapy. Sound waves are bombarded against your heel to stimulate healing within the ligament. This treatment can result in bruises, swelling, pain, and numbness, and has not been proven to be consistently effective in relieving symptoms.

Surgical Treatment
In unusual cases, surgical intervention is necessary for relief of pain. These should only be employed after non-surgical efforts have been used without relief. Generally, such surgical procedures may be completed on an outpatient basis in less than one hour, using local anesthesia or minimal sedation administrated by a trained anesthesiologist. In such cases, the surgeon may remove or release the injured and inflamed fascia, after a small incision is made in the heel. A surgical procedure may also be undertaken to remove bone spurs, sometimes as part of the same surgery addressing the damaged tissue. A cast may be used to immobilize the foot following surgery and crutches provided in order to allow greater mobility while keeping weight off the recovering foot during healing. After removal of the cast, several weeks of physical therapy can be used to speed recovery, reduce swelling and restore flexibility.
Stretching Exercises
Calf stretch. Lean forward against a wall with one knee straight and the heel on the ground. Place the other leg in front, with the knee bent. To stretch the calf muscles and the heel cord, push your hips toward the wall in a controlled fashion. Hold the position for 10 seconds and relax. Repeat this exercise 20 times for each foot. A strong pull in the calf should be felt during the stretch. Plantar fascia stretch. This stretch is performed in the seated position. Cross your affected foot over the knee of your other leg. Grasp the toes of your painful foot and slowly pull them toward you in a controlled fashion. If it is difficult to reach your foot, wrap a towel around your big toe to help pull your toes toward you. Place your other hand along the plantar fascia. The fascia should feel like a tight band along the bottom of your foot when stretched. Hold the stretch for 10 seconds. Repeat it 20 times for each foot. This exercise is best done in the morning before standing or walking.
Work Outs For Broken toes
If your Back Pain feels like a bruise or a dull ache, you may have metatarsalgia People with metatarsalgia will often find that the pain is aggravated by walking in bare feet and on hard floor surfaces. Pain in the ball of your foot can stem from several causes. Ball of foot pain is the pain felt in the ball of foot region. Metatarsalgia is a condition characterized by having pain in ball of foot. The average adult takes about 9,000 steps per day.
If changing your shoes isn't helping to solve your foot pain, it is time for us to step in. Contact Dr. Jeff Bowman at Houston Foot Specialists for treatment that will keep your feet feeling great. Inserting arch support insoles in the shoes is also a good option.
Pain often occurs suddenly and mainly around the undersurface of the heel, although it often spreads to your arch. The condition can be temporary, but may become chronic if you ignore it. Resting usually provides relief, but the pain may return. Heel spurs are bony growths that protrude from the bottom of the heel bone, and they are parallel to the ground. There is a nerve that runs very close to this area and may contribute to the pain which occurs.

Another solution is to wear custom foot orthotics, like ezWalker ® Performance Custom Orthotics, in your shoes to help correct your body posture, stabilize your balance, relieve pain during follow-through and evenly redistribute your weight on your feet. EzWalker® Custom Orthotics are specifically made for each of your feet to properly support your arches while reducing pressure on the balls of your feet. With ezWalker® Custom Orthotics, you'll walk from lateral heel to medial forefoot for better biomechanics of your entire body. This condition manifests as a skin lesion that assumes a ring-like pattern. It can affect any region of the body, right from the scalp to the foot. One such common home remedy is the use of bleach. Many people claim that this is a very effective ringworm treatment.

During the average lifetime our feet cover over 70,000 miles, the equivalent of walking four times around the world., so it's not surprising that problems can occur. Indeed around three-quarters of all adults will experience some sort of problem with their feet at some time. And without treatment most foot complaints will become gradually worse with time. This means people often endure painful conditions for far too long, and the problem can get worse. People often assume nothing can be done to help their condition, but in fact these conditions are extremely treatable. Swollen lump on big toe joint; lump may become numb but also make walking painful.
Limb Lengthening News
Limb Lengthening News
Sun, May 16,2004
Operation'ssomewhat of a stretch
Growthin leg-lengthening surgery for cosmetic purposes dividing doctors
ByJENN GEAREY, Ottawa Sun
Itis said that good things come in small packages but when it comesto being small in stature, some people are going to painful lengthsto make themselves taller. Cosmetic leg lengthening is a surgicalprocedure gaining in popularity. Traditionally, it's been performedon children to correct disproportional leg lengths or to repair aleg after an accident. It's also been an option for people with dwarfism.
Butnow some people are seeking the operation for esthetic reasons, andpaying close to $100,000 for a couple of extra inches.
Ottawanative Dr. Dror Paley, co-establisher and co-director of the LifebridgeInternational Center for Limb Lengthening in Baltimore, Md., has beenperforming leg lengthening surgeries for more than 18 years. He saysonly about 5% of his patients have the surgery for cosmetic reasonsand there are rules about who can have it done.
"Ourcutoff, which is fairly arbitrary, is 5-foot-7 for males and 5-foot-2for females," says Paley. "One really has to question why we havea limit. There's no more danger to someone 5-foot-9. It's more ofan ethical question.
'HEIGHTNEUROSIS'
"Mostof the people who want this done are suffering from a psychologicalcondition which we call 'height neurosis' or 'height dysphoria.' Youcan have height dysphoria being 5-foot-11 so it's not related to youractual height, it's a psychological condition and it's one of thefew psychological conditions you can correct with surgery. The issueis that it's a big surgery and it's a risky surgery and in our handsit's very successful, but in the hands of most people it's fairlydangerous."
Manyleg lengthening patients are private about their operation and oftengo to extraordinary lengths to ensure no one finds out.
"Theyinvent incredible stories to avoid people knowing they're going throughit," says Paley. "One guy told people he was going on a ski trip andthen he had an accident and both of his legs were broken and had tobe fixed. Somehow, when he got out of the wheelchair, he was threeinches taller!"
Typically,patients are men in their 20s, 30s and 40s who are intelligent andwell-adjusted but feel their short stature adversely affects theirlife.
"There'sa tremendous amount of intrigue about it," says Dr. Robert Rozbruch,director of the Institute for Limb Lengthening and Reconstructionat the Hospital for Special Surgery in New York. "I've had many inquiriesfrom patients from Canada ... I get about 20 to 30 e-mails a monthfrom people about cosmetic limb lengthening.
DOLLARINCENTIVE
"Thedeterrent right now is not the pain or the time, it's the dollars.If it were something that was less expensive, or something coveredby the insurance companies, we'd be doing five times as many of these."
Butnot all orthopedic surgeons trained to do the operation agree withperforming it for cosmetic reasons.
"Basically,you're taking a healthy, normal leg and doing surgery on it for cosmeticreasons and some of the risks of cosmetic lengthening are the potentialfor infection in bone, and nerve and blood vessel damage," says Dr.Robert Feibel, an orthopedic surgeon at the Ottawa Hospital, who hasbeen performing leg lengthening for medical, non-cosmetic reasonssince 1993.
"WhileI did my training in Italy there was a patient who was being treatedwho had both of his femora lengthened," says Feibel. "One side waslengthened 10 cm and on the other side the mechanism failed and heonly lengthened 1 cm."
Withan average height gain of only two to three inches, doctors like Feibelquestion whether the cosmetic procedure is really worth a patient'spain and suffering.
Thecurrent method used in the majority of leg lengthening patients --and used in the U.S. for more than 15 years -- is called the "Ilizarov"method. And according to doctors and patients, the severe pain sufferedduring recovery doesn't compare to the dull pain typically associatedwith cosmetic surgery.
Withthe Ilizarov leg lengthening method, a psychological evaluation isusually first conducted to ensure the patient can endure the lengthyrecovery ahead -- up to a year in a wheelchair.
Ifthe patient is psychologically suitable, in a two-hour surgical procedurethe tibia and fibula bones in both legs are broken. On the legs, smallholes are drilled through the patient's skin and an external fixatordevice that consists of metal rods is attached to each half of eachsevered bone using pins and wires.
Lengtheningof the legs begins about a week after surgery and continues over thenext three months. New bone growth is achieved as a result of thepatient turning a variety of screws in their legs which graduallyincreases the distance between the bones and allows new bone growthto occur in the space between.
Onaverage, the patient gains 1 mm of height per day and is requiredto do up to two hours of physical therapy every 24 hours. Althoughphysical therapy is extremely painful, not performing it can extendfull recovery by years. Doctors say that most leg lengthening patientsrequire a narcotic to deal with the intense pain, although this kindof medication often also slows the healing process.
'OPENWOUNDS'
Six-foot-tallJordan Taylor, 19, a Carleton Place high school student, didn't needthe leg lengthening procedure to enhance his height. But in 1996,after a car accident broke the growth plate in one of his legs, itdidn't grow as long as it should have. Two weeks ago, Taylor optedfor the leg lengthening surgical procedure with Feibel.
"Thebiggest problem with this surgery is that you have open wounds thewhole time so they're prone to infection," says Taylor. "It's onlytwo weeks in and I already have one."
ButTaylor says that's to be expected -- and so is some pain that willaccompany tightening the screws in his legs every three hours, whichbegins this week for him.
"SinceI'm tightening the bolts in such small increments I shouldn't havemuch pain, but the physiotherapist at the hospital said I'd betterbe on pain medication when I start turning them," says Taylor.
Infive to nine months, when a patient like Taylor achieves newly grownbone that's strong enough to bear their body weight, they will nolonger need a wheelchair. The last step will be to perform an operationto remove the external fixator device on the leg.
Formost patients the leg lengthening procedure ends here but, in cosmeticcases, some people opt for a second operation to gain even more height.This time the femur bones of the thighs are broken and lengthenedusing the same procedure, giving the patient an additional three inches.Many doctors oppose this, as an additional six inches in the legs-- three on the lower legs and three on the upper -- will likely makethe person appear significantly disproportional.
Butnew methods of leg lengthening surgery are now emerging, facilitatingthe lengthening by omitting the need for any external devices, cuttingthe recovery time and catching the eye of many orthopedic surgeons.
"There'sa metal rod that's telescopic that attaches to the bone inside theleg and the patient literally just shakes their leg and the shakingof the leg moves the rod, which translates into lengthening," saysPaley about ISKD, a new method currently in trials.
Leglengthening doctors strongly advise that potential patients be extremelyvigilant with whom they choose to perform any leg lengthening operation,as inexperienced doctors could cost the patient their legs for life.
"Peopleshould have the right to have surgical procedures to alter their bodies,but you're making an assumption that the surgery is done reliablyand safely," says Paley.
'FEWSURGEONS'
"Atthis point, very few surgeons can carry this out in a reliable, safemanner and achieve the kind of results that we get. Lengthening itselfhas a lot of potential complications and how to treat or prevent thepotential complications of lengthening is where the main knowledgeis required, which is what most people don't have."
Althoughcosmetic leg lengthening is performed in a variety of countries otherthan the U.S., including China, Egypt, France, Germany, Greece, India,Italy, Jordan, Iran, Russia and the Ukraine, U.S. surgeons warn: Buyerbeware.
"They'redoing it in foreign countries, but I've seen some mess-ups. I've hada patient who was operated on in Greece because he got a really goodprice, but it was done by people who really didn't know what theywere doing," says Rozbruch.
Althoughan orthopedic surgeon practising in Canada has yet to offer cosmeticleg lengthening, Feibel hasn't dismissed the idea for the future."With conventional Ilizarov surgery, I don't think it's the rightthing to do right now," says Feibel. "But certainly the internal fixationlengthening (like the ISKD method) will change the approach to cosmeticlengthening and there may be some surgeons who may begin doing it.
"I'veseen two patients in the past who have come to me about cosmetic lengthening,but after reviewing the risks with them they've elected not to doit," says Feibel. "The most important thing to remember is that wedon't have long-term data to show this is a safe treatment. 'Caution'is the word for any cosmetic lengthening -- we really need to seewhat the 10- and 15-year followup is like."